Introduction
A fracture of the 5th metatarsal bone is a specific problem of people who are permanently exposed to foot overload, including athletes. Fractures most often affect the base of the 5th metatarsal and make for 40 to 75% of all foot fractures (Wang et al., 2020). The challenge often is the diagnosis itself, and most notably determining the correct type of the fracture. The literature concentrates on a few particular divisions of 5th metatarsal fractures, the most popular of which seems to be the one proposed by Lawrence and Botte (1993). They differentiate between three types of fractures in the proximal part of the 5th metatarsal bone: the tuberosity avulsion fracture, the Jones' fracture and the proximal diaphyseal stress fracture.
An avulsion fracture is an injury which occurs as a result of a rapid pull (usually the consequence of a sudden stop), a fracture emerging near the epiphysis of the bone along with a bone fragment detachment (Bowes and Buckley, 2016).
Stress fractures are the fallout of the accumulation of overloads which are not able to cause injury independently, but their multiplication leads to weakening of the bone tissue and in consequence, to its fracture. Stress fractures mainly affect the shaft of the bone (Mayer et al., 2014).
Some discrepancies may be found due to diverging definitions of Jones fractures among different authors (Baumbach et al., 2017). Basically, this type of the fracture relates to an injury approximately 1.5 cm from bone tuberosity. In this zone both acute and stress fractures occur. The main reason of increased probability for a stress fracture in this area is its very limited blood supply. This could be the reason for reduced regenerative capacity of the bone tissue in this particular spot, which makes it difficult for micro-injuries to regenerate. Restricted internal hip rotation, evidence of varus hindfoot alignment and field surface are subsequent factors which increase the risk of this fracture (Miyamori et al., 2019; Raikin et al., 2008; Saita et al., 2018). A low level of agility and motor control also play the key role in injury occurrence (Borghuis et al., 2008).
Soccer, due to its requirements of covering up to 12 000 m in a game, frequent changes of direction and a multitude of various incidents (including fouls), seems to significantly increase the risk of foot injuries, including fractures among players (Boraczyński et al., 2020). The player's position on the field has to be considered in this regard (Thomson et al., 2018).
X-ray imaging is usually sufficient in the diagnosis of acute fractures. Problems can be caused by an incorrect diagnosis in the early stages of stress fractures, as they may not be clearly visible in X-ray imaging. MRI or skeletal scintigraphy are recommended in cases of lateral foot tenderness that worsen during exercise, which is one stress fracture symptom. Ultrasound examination is a cheaper and equally useful method of diagnosing stress fractures of the 5th metatarsal bone. They can be all used both in the diagnostic process and monitoring of bone union (Battaglia et al., 2013).
The therapy depends on the type of injury and the physical activity of the patient. Minor fractures without bone dislocation are treated conservatively through temporary immobilization of the limb (6 to 10 weeks). A surgical intervention is recommended for more serious injuries, delayed union and non-union injuries (Miller et al., 2019; Pecina et al., 2011).
In sports medicine, the preferred treatment method of almost all fractures of the 5th metatarsal bone is a surgical anastomosis, which results in a lower no-growth rate, shorter healing time, faster recovery and better clinical outcomes compared to conservative treatment (Bernstein et al., 2018).
The main purpose of the study was to determine the minimum amount of time necessary for a permanent return to the sport after a 5th metatarsal fracture among professional soccer players.
Methods
A retrospective review of a database of professional soccer players from the Polish league who underwent surgical fixation of the 5th metatarsal fracture between January 2014 and June 2019 in one orthopedic center was performed. A person having at least four training sessions a week for at least three years and who had played in the Polish soccer league (Ist and IInd divisions) matches was considered a professional player. Information on age, sex, affected side, body mass index (BMI), and injury mechanisms was collected from the hospital's electronic database. Twenty-one soccer players who underwent surgical anastomosis of the 5th metatarsal with a cannulated screw were included in the evaluation (Figure 1). The inclusion criteria were as follows: a professional Polish soccer player; age between 16 and 35 years; an acute, isolated and closed fracture of the 5th metatarsal bone with a cannulated screw fixation, a follow-up over 12 months. The exclusion criteria were: age under 16 years; a follow-up less than 12 months; open or inveterate fractures; multiple fractures; incomplete chart or radiographic records. The characteristics of all participants are presented in Table 1. The average age of players was 23 (± 4) years, and their BMI was 23 (± 1.2). All patients underwent standard percutaneous internal fixation with the use of a cannulated screw. Return to play (RTP) was determined on the basis of medical records and defined as a return to full training loads.
Figure 1
X-ray of the fifth metatarsal fracture in left foot in an elite soccer player: A-lateral, before surgery; B- anteroposterior, before surgery; C-anteroposterior postoperatively after open reduction

Table 1
Participants’ characteristics
Standard percutaneous internal fixation with cannulated screws using spinal anesthesia was performed on all patients included in the study. The metatarsal base was approached through a dorsolateral incision followed by rhomboidal dissection. The section between the short and long fibular tendons was used to arrive at the bone area. The fixation was preceded by the Kirschner wire insertion into proximal tuberosity. A cannulated screw was fixated as soon as satisfactory positioning was achieved. The final objective was rigid fracture fixation with compression of the top. The postoperative protocol is presented in Table 2 and was similar for all patients.
Table 2
Postoperative rehabilitation protocols
Players were divided into two groups: Group A - only players who underwent surgical treatment (n = 11), Group B - players who underwent conservative treatment first, and surgical treatment due to nonunion or refracture (n = 10). Group B was divided into two subgroups: 1 - players with a nonunion bone and with modification of the treatment type (n = 4), 2 - players who returned to play after conservative treatment and had subsequent injury in the same bone (n = 6). The reinjury and nonunion bone cases were treated surgically using a cannulated screw.
Statistical analysis
The data analysis revealed that all data were normally distributed, with no further transformation required. A t-test was applied to compare time needed to RTP and total inability to play between groups. ANOVA was used to determine interactions of age, weight, height and BMI on their effect on the fracture risk. The level of significance was set at p < 0.05 and all data were expressed as mean ± SD.
Results
Midfielders were prominent in the group of risk for the fracture and comprised 48% of the examination group. A single patient from Group A suffered bone refracture. The cause of this injury was a foul by a player of the opposing team four weeks after RTP.
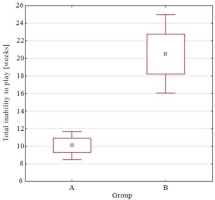
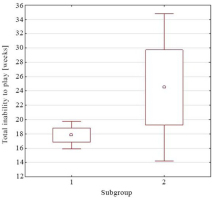
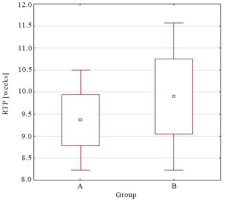
RTP after surgery was on average 9.5 (± 2.3) weeks. Time between the surgery and RTP in group A was 0.4 weeks shorter than in group B (9.3 vs. 9.7 weeks; p > 0.05) (Figure 2). The longest time need to RTP after surgical treatment was reported for players in subgroup 1 (10.8 ± 3.1 weeks). Average time between RTP after conservative treatment and a refracture was 21.7 (min 6; max 52) weeks. A total time of inability to play was 10.3 (± 2.8) weeks in Group A and 20.5 (±7.2) weeks in Group B (Figure 3). The longest period of inability to play was in Group A, and concerned a player who suffered from a refracture (2 x 8 weeks). In group B, the longest time of absence was reported in a player with a nonunion bone (40 weeks). The total time of inability to play in subgroup 1 was 17.8 (±2.4) weeks and 24.5 (±10.5) in subgroup 2 (Figure 4). There were no statistical correlations between the fracture and age, weight, height.
Figure 2
The time needed to return to play after surgical treatment of the fifth bone fracture - A only surgical treatment players (n = 11), -B players with conservative treatment in the past and surgical treatment next (n = 10) (p > 0.05).
Discussion
Lower limb injuries, including fractures of the 5th metatarsal bone base, constitute a serious problem which can exclude a player from play for several months and significantly affect the athlete’s career. Therefore, the likelihood of experiencing this particular fracture should be minimized, and if it occurs, appropriate steps should be taken as fast as possible to return to full training and performance. One should be aware that the selection of an approach to the injury treatment impacts the quality and time of returning to play. The risk of this exact injury may be related to the profile of the player, the position on the field and the type of training adequate for his/her field position. It has been shown that midfielders are more likely to have their metatarsal bone damaged, and the presented outcomes on this issue are consistent with the literature data (Thomson et al., 2018).
Surgical treatment of acute 5th metatarsal bone fractures brings much better and faster results of recovery compared to conservative treatment (Bernstein et al., 2018; Hong et al., 2018; Japjec et al., 2015). Such a guideline is included in almost every fracture treatment protocol regarding athletes’ convalescence (Japjec et al., 2015). The results presented in our paper confirm this observation. Although there were no significant differences in the time between surgery and RTP in the two groups, there was a more frequent refracture and nonunion bone in conservative treatment patients. About 30% of the study group who underwent conservative treatment in the past experienced a refracture. After surgical treatment, only one refracture was reported (due to an opponent's foul). A higher recurrence rate in the group with conservative treatment, especially athletes, has also been reported in other studies (Wu et al., 2018; Yates et al., 2015). Another problem is the nonunion bone rate, which ranges from 11 to 50% considering conservative treatment (Yates et al., 2015; Valkier et al., 2020). Our study presents four cases (19%) of a nonunion bone after conservative treatment and no such a case after surgical treatment. The average time to RTP after a 5th metatarsal fracture is approximately 9 weeks (Pecina et al., 2011), which was also confirmed in our study. Premature weight bearing on the limb can lead to delayed bone unification and other complications. Miller et al. (2019) showed that players who returned to the game after less than 8 weeks after the injury did not reach full bone union on the radiological imaging. In our analysis we included two cases with shorter RTP time, i.e., 6 weeks, however, no side effects occurred. The lack of statistical correlation between the fracture and age, weight and height may be due to the homogeneity of the group. All patients were professional players, similar in age and body measurements.
The goal of surgical treatment is anatomical reconstruction of the bone structure, which allows for the correct distribution of influencing forces and the adequate biomechanics of the entire foot to be restored (Kadar et al., 2015). While deciding for surgical treatment, the doctor has a choice between several techniques. These include, among others: intramedullary screw fixation, plate fixation and fixation with Kirschner wire (Baumfeld et al., 2015; Huh et al., 2015). The role of the fixation is to guarantee the stability of the broken bone fragments such that distribution of mechanical stress does not induce deformation in the unification area (Porter et al., 2009). The most commonly used method of fixation is intramedullary screw placement under X-ray control from the proximal side of the 5th metatarsal bone towards the lateral part. This technique enables the recovery of the patient’s gait and ability to run within a few weeks after the fixation (Bernstein et al., 2018; Duplantier et al., 2018). A less common solution is a method using Kirschner wire alone, which is the least invasive technique, but at the same time seems to be insufficiently stable, especially in professional athletes (Zwitser and Breederveld, 2010). A plate fixation is characterized by very good endurance and functional performance (Duplantier et al., 2018; Xie et al., 2017). Unfortunately, it is burdened with drawbacks such as a relatively large surgical wound (compared to other methods), the related complications of wound infections and discomfort caused by protruding elements of the plate and screws (Xie et al., 2017). The natural evolution of operational methods from more invasive and less stable to barely invasive and more stable was confirmed by recent reports describing the F.E.R.I. (5th metatarsal, Extra-portal, Rigid, Innovative). It is a synthesis of a stable intramedullary anastomosis with a safe margin of its dynamization. This method seems very promising, yet requires further confirmation of its effectiveness in clinical trials (D'Hooghe et al., 2019). In sports practice, the highest priorities are permanent fusion and comfort of the player's daily function. It is important that the material does not widen the foot contour, which could cause the injured site to become tender while having sports shoes on. Hence, most methods rely on intramedullary fracture fixation (Huh et al., 2016) as it seems to be the optimal choice among the available methods (Japjec et al., 2015). External fixation methods in the form of plate or suture cerclage are not very common due to mechanical discomfort (Huh et al., 2016; Mofidi et al., 2009; Sarimo et al., 2006), especially during dynamic activity (Granata et al., 2015; Lee et al., 2011).
A necessary addendum to rehabilitation protocols is properly arranged motor control training, which allows to reduce the likelihood of a refracture. In the fast return to sport after a 5th metatarsal fracture, the early fracture stabilization surgery is recommended for athletes, enabling the implementation of an aggressive rehabilitation protocol as soon as possible. Looney et al. (2020) indicated that early limb loading after surgery (from week 2) did not delay fracture healing, nor hinder the bone union. As a result, it shortened the time of absence from training to a minimum, which is very important for professional athletes (Looney et al., 2020). A helpful tool recommended in the early stages of rehabilitation is the external bone stimulator (e.g. Exogen), which shortens the time of bone regeneration and remodeling (Nolte et al., 2016; Teoh et al., 2018). Implementing early conditioning, gait re-education and subsequent running are possible due to an anti-gravity treadmill (Alter G), which is gaining more popularity in innovative rehabilitation protocols (Thomson et al., 2018). During the last phase of rehabilitation and in the programming of sports training, the player's position on the pitch should be taken into account. According to the researchers' findings, non-linear running accumulates greater forces on the inside foot (Thomson et al., 2018). Performing long passes during the game may significantly increase the loads on the lateral side of the foot. Some authors also report that soccer shoes tend to increase the load born on the foot’s sole (Blanchard et al., 2018). After returning to sport, continuous monitoring of the athlete and appropriate management of training loads are recommended, and any pain symptoms should be immediately reported to the medical staff and never be ignored (Kuzuyama et al., 2019; Thomson et al., 2018).