Introduction
Post-exercise recovery has been largely investigated in athletes including the water immersion (WI) modality as a simple and efficient method for restoring cardiovascular homeostasis. Heart rate variability (HRV) is widely used to assess cardiac autonomic modulation and has become an indicator of overall recovery in team-sport athletes (Lukonaitienė et al., 2020; Stanley et al., 2013; Thorpe et al., 2017). However, benefits of WI to cardiac parasympathetic reactivation have received little attention considering female players.
In team sports, the WI recovery modality is widely used during congestive training schedule (i.e., overload period) to minimize fatigue and improve recovery. Thus, practical recommendations for WI based on individual characteristics (e.g., gender) and protocol (i.e., temperature, duration, type) have been recently proposed (Tavares et al., 2018) for team sports athletes. When cold-WI is prescribed during longterm training periods, controversial effects have been reported (Broatch et al., 2018). While it increases the genetic expression of mitochondrial synthesis after endurance training, it may limit muscle protein synthesis following strength training. When cold-WI is used during the acute post-exercise recovery, benefits are usually attributed to vasoconstriction effects, subsequent reduction in inflammation response, and reductions in ratings of perceived exertion and muscle soreness (Broatch et al., 2018; Ihsan et al., 2016). In response to thermal stress, efferent responses controlled by the higher brain centers (primarily the preoptic hypothalamus) occurred including changes in the cutaneous blood flow (Ihsan et al., 2016). In addition, the integrated cardiovascular responses to cold exposure involve adjustments in autonomic activity which may modulate cardiac output. Given that cold exposure influences the autonomic nervous system, post-exercise cold-WI may involve modulation of cardiac autonomic activity. Studies analyzing the effect of various post-exercise WI modalities at the sinus node step (Al Haddad et al., 2010; Almeida et al., 2016; Buchheit et al., 2009; Choo et al., 2018; de Oliveira Ottone et al., 2014; Stanley et al., 2012) reported that cold-WI was more effective than hot-WI and thermoneutral-WI at increasing cardiac parasympathetic reactivation following exercises. Few studies have analysed the sensitivity of HRV following the contrasting hot- and cold-WI modality. A study reported that contrasting-WI increased post-exercise parasympathetic response to a greater extent than passive recovery, and less than cold-WI (Stanley et al., 2012). Physiological responses to contrasting-WI are not as well characterized as those responses induced by cold-WI (activation of cold receptors in the skin and veins). It seems difficult to predict occurrence of cardiac sympatho-vagal interaction. Finally, benefits of post-exercise WI to HRV have received little research attention during intense training in team sports and particularly in female players (Broatch et al., 2018).
Training camps are usually a part of the preparation period for the regular season and international events in team sports (Flatt et al., 2017; Lukonaitienė et al., 2020; Ronglan et al., 2006). Since athletes are required to achieve their best performance throughout the training camp, they face intense physical activity under mentally stressful situations. The HRV modulation has been considered as a physiological indicator reflecting the training readiness status (Lukonaitienė et al., 2020; Thorpe et al., 2017) and the recovery process (Stanley et al., 2013). The monitoring of post-exercise HRV provides information on the return to homeostasis following strenuous exercises. In that way, derived parasympathetic HRV indices have been related to exercise-induced physiological disturbance during recovery (temperature, plasma epinephrine, blood lactate and pH) (Ihsan et al., 2016). The magnitude and duration of parasympathetic disruption during recovery appeared to be related to exercise variables (i.e., intensity, duration and modality) and individual characteristics (i.e., physical fitness, recovery potential, mood state) (Kaikkonen et al., 2010; Michael et al., 2017; Nakamura et al., 2016; Seiler et al., 2007). The time course of parasympathetic recovery has been widely analyzed to assess the responsiveness of the autonomic nervous system and to reflect indirectly the overall recovery status of players (Ravier & Marcel-Millet, 2020; Stanley et al., 2013). During intense training, the importance of maintaining a high level of parasympathetic activity to trigger positive adaptations was reported (Nakamura et al., 2016, 2018). Adequate periodization of training loads may be one of the solutions. However, during the training camp which lasted no more than two weeks, training load modulation remained limited. In this context, the implement of post-exercise WI may help players improve their HRV recovery.
It is somewhat surprising that the acute benefits of various time and temperature WI protocols to cardiac autonomic activity have not been studied sufficiently, especially in elite female players. Specifically with the national team engaged in a short training period before international events, the reactivation of vagal tone may be crucial. When considering an elite team, the short-term period following the end of training sessions implies routines or a medical follow-up requiring a delay before proceeding to the recovery intervention. The purpose of this study was to investigate the effect of three 60-min delayed post-exercise WI protocols on the parasympathetic reactivation during a training camp with U20 national female handball players. Each WI modality (two contrasting hot- and cold-WI sessions and one cold-WI session) followed handball training. An exacerbated vagal tone disruption was expected in response to training sessions. We hypothesized that the cold-WI recovery modality would be the most effective modality for increasing the acute cardiac parasympathetic reactivation.
Methods
Approach to the problem
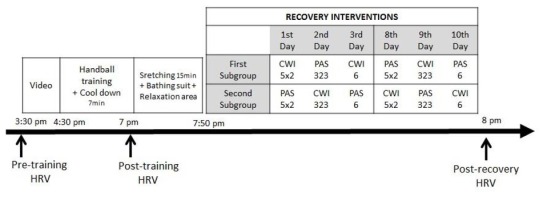
Water immersion is widely used as a recovery modality in team sport athletes. However, benefits of post-exercise WI to HRV have received little research attention in team sports and particularly in female players (Broatch et al., 2018). This study used a controlled crossover design to determine the effect of completing a 60-min delayed post-training WI session compared with no treatment on the cardiac sympatho-vagal balance. The study was undertaken during a genuine field training camp lasting two weeks with females under 20 from the handball national team. Since the training schedule planned by the head coach included similar training intensity volume and daily frequency in the first three days of both weeks, our experiment was conducted during these periods. Three different WI protocols were compared (i.e., each day, one different WI protocol was undertaken) with passive rest (PAS) in a crossover design. One continuous cold session and two contrasting cold- and hot-WI recovery sessions were prescribed in the evening during the first three days of each week. Participants were randomly allocated into a WI or a PAS subgroup. When one subgroup was going through one of the three WI protocols, the other group was involved in the PAS for a similar amount of time. The following week, the subgroups reversed the conditions. Moreover, both WI and PAS subgroups reversed for each subsequent day. Figure 1 provides a schematic view of the experimental protocol. Actually, to allow all players to benefit from the recovery baths throughout the training camp, the PAS subgroup completed the prescribed daily WI modality after ending the experimental evaluations. This additional sequence did not influence the outcomes of our study.
Figure 1
Schematic representation of the experimental protocol in the function of time. HRV, heart rate variability; CWI6, 6-min cold-water immersion; PAS6, 6-min passive recovery; CWI323, 8-min contrast cold- and hot-water immersion; PAS323, 8-min passive recovery; CWI5×2, 10-min contrast cold- and hot-water immersion; PAS5×2, 10-min passive recovery.
Short-term measures of HRV were recorded before and after the late afternoon handball training session, and after the delayed post-training recovery intervention. The pre-training data were considered as a baseline value. In order to determine the physiological demand for handball training sessions, the total group of players was compared before and after each handball session irrespective of subgroups. To investigate the cold-WI effect, each WI modality was compared with its respective passive recovery session.
Participants
Eighteen elite female handball players (mean ± SD: age 18.8 ± 0.4 y, range 18.1−19.4 y) belonging to the French under 20 national team participated in the study. The experiment was carried out during a training camp (11 days) held at the end of the competitive season, four weeks before the women's U20 European Handball Federation Championship. Players' anthropometric measurements were as follows: body mass 72.9 ± 10 kg; body height 177.2 ± 7.5 cm; body mass index 23.1 ± 1.9 kg∙m-2; and body fat content 22.1 ± 3.1% (from the biceps, triceps, subscapular and suprailiac skinfold measurements as described by (Durnin & Rahaman, 1967). Each participant was medically screened throughout the entire season and the training camp, and had no medical or orthopedic problems. All participants were informed of the benefits and potential risks of the investigation. Players received comprehensive verbal and written explanations of the study and provided voluntarily signed informed consent. This study was approved by the Federal Board of the Medical Committee and conformed to the recommendations of the Declaration of Helsinki.
Design and Procedures
The training camp included two sessions per day. One prophylactic session and a light training sequence were completed in the morning. At the beginning of the afternoon players could rest up to 3:00 PM, then a video sequence preceded the main daily handball training session. Pre-training HRV measurement occurred immediately before the team video sequence which preceded the handball training session. Training sessions included a warm-up (≃10 min), shot repetitions (≃10 min), team's offensive and defense drills (≃10 min), a playing sequence on the regular handball court with specific tasks involving regular interruptions by the coach (≃40 min), high intensity exercise (≃15 min consisting of intermittent shuttle running or small-sided game) and continuous 20-min match play.
Handball training ended with a 7-min submaximal run to allow an HR steady-state signal required for appropriate short-term HRV analysis (Al Haddad et al., 2010). Thereafter, post-training HRV was recorded. During the subsequent 45 min, players completed stretching, wearing bathing suits and bathrobes, joined the relaxation area, and waited for the recovery intervention. Then, all the participants underwent the recovery interventions (≃10 min, WI or rest) at the same time, which were immediately followed by the HRV measurement. Investigators supervised this period from the end of the handball training session. Handball training and recovery protocols were planned at the same time of the day throughout the training camp. The exclusion criterion was applied for players who did not entirely perform the late afternoon handball training session and/or did not complete the recovery sequence by any circumstance.
The three WI protocols were i) a contrasting water temperature modality with three 2-min periods of cold-WI interspersed by 2 min of hot-WI (CWI5×2), ii) a contrasting water temperature modality including two 3-min periods of cold-WI interspersed by 2 min of hot-WI (CWI323), and iii) one continuous 6-min period of cold-WI (CWI6). Each protocol included a total of 6 min cold-WI. Considering that cold-water temperature was harder to bear than hot water, protocols were undertaken according to the following order to allow a gradual increase in the duration of cold periods: CWI5×2, then CWI323 and finally CWI6 for both weeks. Participants had to go into the water up to the navel. The temperature of cold- (10°C ± 0.5°C) and hot- (34°C ± 0.5°C) pools was automatically adjusted by the controlling system and continuously monitored by a digital display. For the PAS recovery participants rested in a seating position in a relaxation area (22 ± 0.5°C) for the same amount of time as the cold-WI protocol. The temperature of the room was automatically adjusted by the air conditioning system, which was monitored by a digital display.
The participants’ HR was measured before and after the handball training session, and after the recovery intervention which took place at the same time of the day throughout the training camp. Data were collected using a HR monitor (HR1 chest belt, Matsport, Saint Ismier, France) with ANT+ wireless transmission. Participants were recorded all together at the same time using Mooky Center software (Matsport, Saint Ismier, France) which allowed to collect more than twenty signals simultaneously. Immediately after the end of WI protocols, participants wore their bathrobe and went to the adjacent room to start measurements. This procedure took between 2 to 2.5 min. Participants were told to remain seated and breathe spontaneously without speaking or making any movement for 5 min. These instructions were reminded before each HR measurement. The analysis window of HRV indices was 5 min including 1 min of the stabilization period and 4 min of analysis (Bourdillon et al., 2017). The HRV value registered with a sampling rate of 1000 Hz, and the R-R intervals were analyzed using Kubios HRV analysis software, version 3.0.2 (Biosignal Analysis and Medical Imaging Group, University of Kuopio, Kuopio, Finland). The correction level imputed on Kubios software was chosen by visual inspection of the interval tacogram, in a way to ensure that the correction removed the artefacts without distorting the normal R-R intervals. The analysed HRV indices for the time-domain dependent variables were the R-R intervals (RR, ms), the root mean square of the successive differences of the normal R-R intervals (RMSSD, ms) and the standard deviation of the normal-to-normal interval (SDNN, ms). In the frequency domain, analysis included low (0.04−0.15 Hz) frequency (LF) and high (0.15−0.4 Hz) frequency (HF) in normalized units (n.u.). Furthermore, instantaneous beat-to-beat variability (SD1, ms) and continuous beat-to-beat variability (SD2, ms) derived from the Poincaré Plot analysis were analysed. Among HRV indices, RMSSD, HF and SD1 reflect cardiac parasympathetic activity, whereas RR, HR, SDNN, LF and SD2 reflect both cardiac vagal and sympathetic activities (Peçanha et al., 2017).
Statistical Analysis
Data are reported as mean ± SD. The normality and equality of variance were checked using the Shapiro-Wilk’s test and the Bartlett’s test, respectively. When the sample was skewed, data were log-transformed (natural logarithm, ln) to allow for parametric statistical comparison. The acute effect of handball training on HR and HRV indices was tested with two-factors analysis of variance (ANOVA) (week1, week2 × pre-, post-training) with cold-WI and PAS participants altogether (cold-WI + PAS). Moreover, variations from pre- to post-training values were compared between week1 and week2 with a Student-paired t-test. A mixed-design factorial ANOVA was used to determine the significant mean effects on changes over time (pre-, post-exercise and post-recovery) and interaction effects between the recovery conditions (PAS and cold-WI) for HR and HRV indices. Pairwise comparisons were tested using the post-hoc Tukey’s test. Each recovery modality was analysed separately (CWI6 vs. PAS6, CWI323 vs. PAS323, and CWI5×2 vs. PAS5×2). Furthermore, Cohen’s d effect size (ES) (Cohen, 1988) analysis was performed to determine the qualitative difference between recovery conditions (PAS and cold-WI) as well as between time of measurement (pre-, post-training and post-recovery) for all HRV indices. An ES ˂ 0.20 was classified as trivial, 0.20–0.49 as small, 0.50–0.79 as moderate, and ˃ 0.80 as large. The p ≤ 0.05 criterion was used for establishing statistical significance.
Results
The data reported below were obtained for 16 players for CWI5×2 vs. PAS5×2, 13 players for CWI323 vs. PAS323 and 14 players for CWI6 vs. PAS6 after applying the exclusion criterion.
HR and HRV responses to handball training sessions did not reveal differences between the first and the second week for pre-training, post-training and variations from pre- to post-training. However, a significant difference was observed for HR and HRV indices between pre- and post-training values for each individual training session. For the CWI6 + PAS6 modality, the difference between pre- and post-training was significant (p < 0.001 – p < 0.0001, moderate to large ES) with a decrease in lnRMSSD, lnHF, RR, SDNN, lnSD1 and SD2 indices, and an increase in HR and lnLF index. For instance, lnRMSSD was 3.92 ± 0.48 ms pre- vs. 2.91 ± 0.68 ms post-training (p < 0.0001, ES = -1.71, 95%CI = -2.52 – -0.80) for the first week and was 3.78 ± 0.48 ms pre- vs. 3.06 ± 0.63 ms post-training (p < 0.0001, ES = -1.30, 95%CI = -2.07 – -0.45) for the second week. The same trends were observed for CWI323 + PAS323 (p < 0.0001, moderate to large ES) and CWI5×2 + PAS5×2 (p < 0.001 – p < 0.0001, moderate to large ES).
The comparison between CWI6 and PAS6 was the one showing the most significant differences among the three CWI modalities with the interaction effect of time × condition for HR, RR, lnRMSSD, lnHF, lnLF, and lnSD1. Table 1 displays HR and HRV indices at pre-training, post-training and after the 6-min continuous cold-water immersion recovery intervention with qualitative and quantitative comparisons. The comparison between CWI323 and PAS323 is displayed in Table 2. Interaction between moments of measurement and conditions (CWI323 and PAS323) was significant for RR, lnSD1 and lnLF. The comparison between CWI5×2 and PAS5×2 is shown in Table 3. Interaction between moments of measurement and conditions (CWI5×2 and PAS5×2) was significant for SDNN and SD2 (p < 0.05). Table 4 displays qualitative comparison between post-training and post-recovery values for the three WI modalities. Figure 2 summarizes the effect size between pre-training and both post-training and post-recovery for WI and PAS conditions.
Table 1
Heart rate variability indices calculated for the 6-min continuous cold-water immersion modality
[i] Values are mean ± SD and effect size (ES) ± 95% confidence interval (with lower and upper limits). CWI6, 6-min cold-water immersion; PAS6, 6-min passive recovery; Pre-tra, Post-tra and Post-rec, defined the pre-training, post-training and post-recovery time of measurement, respectively. HR, heart rate; HRV, heart rate variability; RR, time interval between R to R waves; lnRMSSD, natural logarithm of the root mean square of the successive differences of the normal RR intervals; SDNN, the standard deviation of the normal-to-normal interval; lnHF, natural logarithm of the high frequency band; lnLF, natural logarithm of the low frequency band; lnSD1, natural logarithm of instantaneous beat-to-beat variability; SD2, continuous beat-to-beat variability. T, effect of time; C, effect of condition; C×T, time and condition interaction following ANOVA.* denotes a significant difference (b = p < 0.001; c = p < 0.0001) between CWI6 and PAS6 after post-hoc analysis following 'time × condition' ANOVA.
Table 2
Heart rate variability indices calculated for the 3-2-3 min contrasting cold-and hot-water immersion modality
[i] Values are mean ± SD and effect size (ES) ± 95% confidence interval (with lower and upper limits). CWI323, contrasting-water immersion; PAS323, passive recovery; Pre-tra, Post-tra and Post-rec, defined the pre-training, post-training and post-recovery time of measurement, respectively. HR, heart rate; HRV, heart rate variability; RR, time interval between R to R waves; lnRMSSD, natural logarithm of the root mean square of the successive differences of the normal RR intervals; SDNN, the standard deviation of the normal-to-normal interval; lnHF, natural logarithm of the high frequency band; lnLF, natural logarithm of the low frequency band; lnSD1, natural logarithm of instantaneous beat-to-beat variability; SD2, continuous beat-to-beat variability. T, effect of time; C, effect of condition; C×T, time and condition interaction following ANOVA.* denotes a significant difference (b = p < 0.001; c = p < 0.0001) between CWI323 and PAS323 after post-hoc analysis following 'time × condition' ANOVA.
Table 3
Heart rate variability indices calculated for the 5×2 min contrasting cold-and hot-water immersion modality
[i] Values are mean ± SD and effect size (ES) ± 95% confidence interval (with lower and upper limits). CWI5×2, contrasting-water immersion; PAS5×2, passive recovery; Pre-tra, Post-tra and Post-rec, defined the pre-training, post-training and post-recovery time of measurement, respectively. HR, heart rate; HRV, heart rate variability; RR, time interval between R to R waves; lnRMSSD, natural logarithm of the root mean square of the successive differences of the normal RR intervals; SDNN, the standard deviation of the normal-to-normal interval; HF, high frequency band; LF, low frequency band; lnSD1, natural logarithm of instantaneous beat-to-beat variability; SD2, continuous beat-to-beat variability. T, effect of time; C, effect of condition; C×T, time and condition interaction following ANOVA.* denotes a significant difference (b = p <0.001) between CWI5×2 and PAS5×2 after post-hoc analysis following 'time × condition' ANOVA.
Table 4
Qualitative comparison between post-training and post-recovery values for HRV indices in cold-water immersion and passive recovery conditions within the three modalities.
[i] Values are effect size ± 95% of the confidence interval. CWI6, 6-min cold-water immersion; PAS6, 6-min passive recovery; CWI323, 8-min contrast cold- and hot-water immersion; PAS323, 8-min passive recovery; CWI5×2, 10-min contrast cold- and hot-water immersion; PAS5×2, 10-min passive recovery. Pre-tra, Post-tra and Post-rec, defined the pre-training, post-training and post-recovery time of measurement, respectively. HR, heart rate; HRV, heart rate variability; RR, time interval between R to R waves; lnRMSSD, natural logarithm of the root mean square of the successive differences of the normal RR intervals; SDNN, the standard deviation of the normal-to-normal interval; HF, high frequency; LF, low frequency; lnSD1, natural logarithm of instantaneous beat-to-beat variability; SD2, continuous beat-to-beat variability. ES, effect size; 95% CI, 95% confidence interval for effect size with lower and upper limits. * specified that raw values were log-transformed when appropriate (i.e., CWI6, PAS6, CWI323 and PAS323)
Discussion
This is the first study monitoring cardiac autonomic response to post-exercise WI with elite female handball players under genuine field conditions. Data confirm that post-exercise parasympathetic disruption was exacerbated due to handball training. The most important finding was the effectiveness of the 60-min delayed post-exercise cold-WI modalities to promote the parasympathetic reactivation.
The present HRV data determined before and during acute recovery following handball training revealed significant exercise-induced HRV modulations. Similar trends were observed daily throughout the training camp with decreases in lnRMSSD, lnHF, RR, SDNN and lnSD1 indices and increases in HR and lnLF index (p < 0.001 – p < 0.0001, moderate to large ES). The magnitude of HRV disruption during acute recovery was marked (Figure 2) regarding the ES for parasympathetic indices (e.g., from -0.8. to -1.7 for lnRMSSD).
Figure 2
Qualitative comparison of HRV indices between times of measurement relatively to pre-training values in WI and passive conditions. Standardized differences (Cohen's d). Data presented effect size ± 90% confidence interval. The gray area denotes a trivial zone.
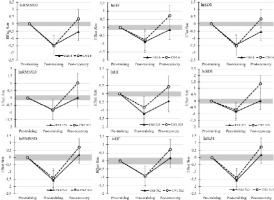
Besides the magnitude of the HRV disruption, the time course needed to recover baseline values is a valuable indicator reflecting the overall recovery status and training load (Kaikkonen et al., 2010; Michael et al., 2017b; Seiler et al., 2007). Figure 2 shows that many HRV indices remained decreased for at least 60 min after the end of handball training (e.g., moderate ES for lnRMSSD and large ES for RR with PAS6; moderate ES for lnHF with PAS323). After various endurance (Kaikkonen et al., 2010; Michael et al., 2017b; Seiler et al., 2007) and team sport (Flatt and Howells, 2019; Ravier and Marcel-Millet, 2020) exercises, previous studies reported that intensity was the exercise characteristic having the greatest impact on delaying post-exercise HRV recovery. The post-exercise cardiac parasympathetic disruption observed was up to 50 min after exercise performed until exhaustion in physically active males (Almeida et al., 2016), and 60 min after a Crossfit® workout in healthy adults (Kliszczewicz et al., 2016). In the present study, both magnitude and duration of HRV disruption demonstrated a dramatic perturbation of cardiac parasympathetic reactivation and sympathetic withdrawal during recovery.
Comparison between the WI modality and passive recovery revealed significant time × condition interaction particularly for the CWI6 modality (Table 1). Actually, comparison between CWI6 and PAS6 was the one showing the most impressive post-hoc results with post-recovery differences for all parasympathetic indices (inferred from lnRMSSD, HF and lnSD1; p < 0.001 – p < 0.0001, with large ES ranging from 0.86 to 0.94). CWI6 was the only one triggering higher parasympathetic activity than passive recovery, which elicited two comments. Firstly, the beneficial effect observed with CWI6 compared with PAS6 was in accordance with previous studies (Al Haddad et al., 2010; Buchheit et al., 2009). For instance, compared with passive recovery, 5-min continuous cold-WI (≈ 15°C) applied immediately following a short supramaximal cycling sprint, increased lnRMSSD values during immersion (Al Haddad et al., 2010) and increased lnHF after (Buchheit et al., 2009) the recovery intervention. However, it seems important to specify that previous studies applied cold-WI strategies immediately or with a short delay (10-20 min) after the end of the exercise. In the present study, the recovery modalities were applied 60 min after the end of training, what was an innovative approach. The effectiveness of delayed CWI6 in triggering greater parasympathetic activity than passive recovery could be described as a "boost effect". Indeed, the adjunction of a short period of WI increased rapidly and noticeably the vagal tone. Secondly, neither CWI323 nor CWI5×2 revealed any difference compared with their passive recovery condition (except for CWI323 with lnSD1, p = 0.049). This might be due to the contrasting water temperature protocol. Even if hydrostatic pressure showed beneficial effect on vagal-related HRV indices (Al Haddad et al., 2010), water temperature is the major factor influencing HRV (Al Haddad et al., 2010; Almeida et al., 2016; de Oliveira Ottone et al., 2014). The acceleration of post-exercise parasympathetic reactivation following cold-WI strategy (15 min at 15° C) was previously reported while 15-min temperate-WI (28°C) or hot-WI (38°C) reduced RR, lnRMSSD and lnSD1 (de Oliveira Ottone et al., 2014). Moreover, the optimal duration recommended for the cold period (14°C) was 15 min (Almeida et al., 2016). Finally, Stanley et al. (2012) reported lower benefits of contrasting-WI (14°C for 1 min + 35°C for 2 min, repeated 3 times) on post-exercise HRV recovery compared with 5-min cold-WI (14°C). The present results demonstrate that neither CWI323 nor CWI5×2 induced a higher increase in cardiac parasympathetic indices than passive recovery.
In respect to the effect size and qualitative descriptor, the comparison between post-training and post-recovery values (Table 4) showed an increase in cardiac parasympathetic indices for the three WI modalities. Despite passive recovery showed large ES (e.g., lnRMSSD ranging 0.89 – 1.67), each WI modality presented higher ES (e.g., lnRMSSD ranging 1.69 – 2.11) than their respective passive recovery for all parasympathetic indices. It is difficult to predict the possible occurrence of cardiac sympatho-vagal interactions when applying cold-WI immediately following the end of strenuous exercise. During recovery, the cardiovascular system facilitates physiological processes, including thermoregulation and removal of waste products. On the one hand, at the onset of recovery high metabolite clearance is requested involving high metaboreflex input (Michael et al., 2017a) which contributes to maintaining the cardiac sympathetic activity. On the other hand, cold-WI increases vasoconstriction which results in decreasing skin and limb blood flows. Then, central blood volume increases and the enhancement of peripheral vascular resistance leads to increased stroke volume and cardiac output. Activation of arterial baroreflex inhibits sympathetic activity and stimulates parasympathetic activation. Based on ES, the present study showed a higher decrement in HR and lnLF following post-exercise WI than passive recovery with concomitant benefit to the cardiac vagal tone. It seems reasonable to assume that 60-min delayed post-exercise WI contributed to the agonist response of sympatho-vagal balance.
Finally, the post-recovery values expressed relatively to pre-training showed unexpected trends (Figure 2). Most of parasympathetic HRV indices revealed higher values after WI than pre-training (i.e., baseline). The pre-training measurement was implemented after a moment of rest, but just before starting the video sequence (Figure 1). Firstly, the lower baseline values might be associated with psychological stress resulting from the context of the international tournament preparation phase, i.e., feeling of anxiety before selection combined with the willingness to perform the best during all training sessions. Secondly, the video sequence following immediately the HRV measurement might influence vagal-related HRV indices. Indeed, concentration needed to understand tactics and stress resulting from coaches' feedback on individual and collective behavior should induce an additional psychological load. Previous studies reported a relationship between the vagal tone, emotional regulation and cognitive skills. In soccer, it has been reported that a 30-min period of demanding cognitive activity increased the perception of mental fatigue (Smith et al., 2016). Cognitive tasks increased both α-adrenergic (vascular) and β-adrenergic (cardiac) sympathetic activity (Mestanik et al., 2015). In the health field, stressful situations involved low parasympathetic activity which increased the LF and decreased the HF band (Kim et al., 2018). In the present study, pre-training HRV data may be related to current psychological stress, higher cognitive skills and better capability to engage in the activity. Regardless of the underlying mechanism, delayed post-training cold-WI promoted the improvement in the parasympathetic HRV indices compared to the pre-training values.
This study has several strengths. First, the experiment occurred during a genuine field training camp with female handball players. Moreover, the 60-min delay between the end of training/match and cold-WI respected the real field conditions with team sports players. However, despite the present study demonstrated a positive effect on parasympathetic activity recovery considering pre-training values for CWI6, it was not investigated how this effect would carry over to the next training session. A previous study reported that 15-min cold-WI had short-lasting effects with no evidence four hours after the recovery intervention (de Oliveira Ottone et al., 2014). Nevertheless, it was recently reported that 3-min whole body cryotherapy completed during recovery in the evening promoted the quality of sleep and improved the parasympathetic tone during night (Douzi et al., 2019). This promising result gives prospects to test the reliability between the "boost effect" currently observed in response to CWI6 and the quality of sleep.
In conclusion, this study highlights that post-exercise parasympathetic disruption was intensified due to handball training. The most important finding is that a 60-min delayed post-exercise WI strategy is efficient in increasing the parasympathetic activity beyond the basal values. Finally, CWI6 demonstrated higher improvement in the cardiac vagal tone compared with passive recovery.


